If you are having trouble conceiving, you might have heard about intrauterine insemination, or IUI for short. IUI is a popularly used fertility treatment to increase the chances of pregnancy as well. However, IUI might not be a good ‘fit’ for you, and this article will cover the details of ‘what is IUI’ and ‘how it works’ as well as go into detail about who it is ideal for. The information shared will help you and your family understanding IUI if you should go for IUI or not.
What is IUI? Understanding IUI
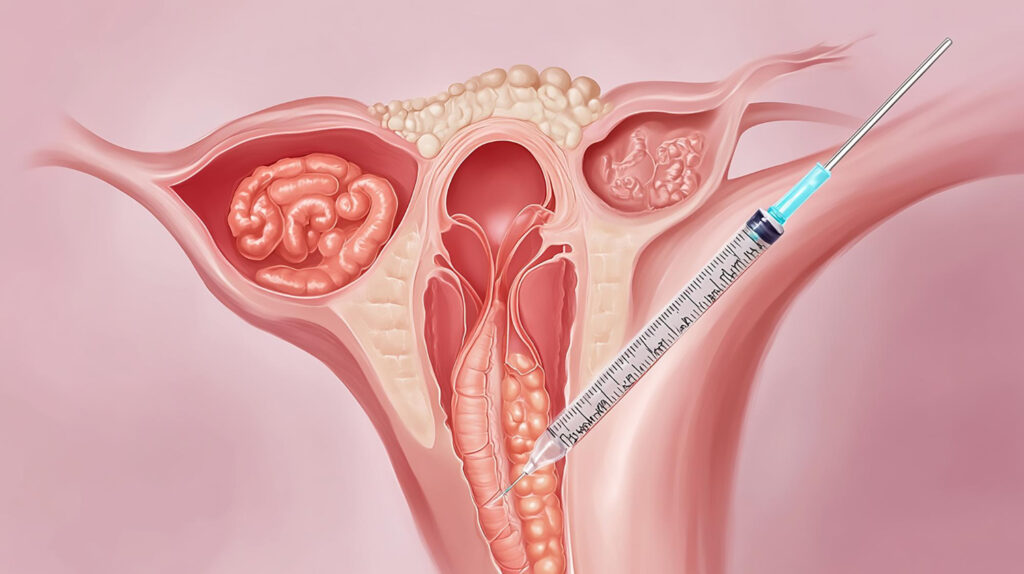
IUI is using sperm and placing it directly in a woman’s uterus during her ovulating period. This process, IUI, is used to bypass the use of cervical mucus, which increases the chances of sperm swimming toward the egg and creating a baby.
The procedure involves tracking the woman’s ovulation cycle, and doctors have a better opportunity to use fertility medications to stimulate the woman’s ovaries through this. After proper steps are taken, they collect a sperm sample. This might either come from your husband or a sperm donor. The sample is processed in a laboratory and inserted into the uterus through a thin tube until the egg gets fertilized.
Who May Require IUI Treatment?
IUI is helpful for individuals and partners facing some form of infertility. Here are examples of infertility conditions that make IUI a favorable option:
Ovulatory Disorders
Women suffering from anovulation or ovulation disturbances may be advised to use IUI for better chances of conceiving. Clomid and other fertility drugs can induce ovarian activity, which can facilitate the timing of the IUI.
Male Infertility
IUI is a perfect option when the male has a low sperm count, low sperm motility, or abnormal morphology. It is equally restrictive for male infertility that one has to undergo multiple natural barriers before the egg is even fertilized. With IUI, sperm is injected deep into the uterus, so many of the obstacles to conception are avoided.
Unexplained Infertility
When the cause of infertility is unknown, IUI can also be the initial treatment one physician recommends. Infertility, in this case, is even more complicated than unexplained, where all factors are present, but for some reason, the child is not conceived. IUI serves as an enhanced mechanism for the deposition of the sperm with the egg strand such that warring conditions to fertilization are minimized.
Sperm Donor Use For Single And Same-Gender Couples
IUI is an option for single heterosexual women, single same-sex women, and married women who want to have a baby. The techniques remain the same, except that a donor chosen from a sperm bank is used.
Everything You Need to Know About the IUI Procedure
In preparation for IUI, patients retrieve fertility assessments comprising blood work, ultrasound, and semen analysis, among other tests. The procedure lasts for a few minutes and doesn’t involve anesthesia.
Step 1: The Doctor Keeps Track Of Your Ovulation Cycle
The accurate timing of the IUI is critical. As a result, your practitioner will monitor your ovulation cycle. This will require ultrasounds and blood tests each month to track the follicle development. The cycle tracking will determine when you’re scheduled to get the IUI, as it is most effective during or right before ovulation.
Step 2: Preparing the Sperm
After scheduling you for an appointment, your practitioner will collect a sperm sample around the time you’re ovulating. The sample is then screened, tested, and prepared at a nearby laboratory, and the most active and healthiest sperm is sorted out. This procedure is essential because it increases the likelihood of fertilization.
Step 3: Transferring the Sperm To The Uterus
During the IUI procedure, a thin tube, also known as a catheter, is used to inject sperm into the uterus through the cervix. The transferred sperm can then swim up the fallopian tubes to fertilize the egg. The process takes less than 20 minutes and can easily be integrated into daily activities.
Success Rates of IUI: What to Expect
IUI is not a guaranteed solution, but many couples experience success with this treatment. Success rates can vary based on several factors, including the woman’s age, the cause of infertility, and the number of IUI cycles attempted.
In general, IUI success rates range from 10% to 20% per cycle. For women under 35, the chances of success are higher. However, for women over 40, success rates tend to decrease. It’s important to have realistic expectations and work closely with your fertility specialist to determine the best course of action.
Factors That Affect IUI Success
- Age: Younger women typically have higher success rates with IUI.
- Sperm Quality: The quality and quantity of sperm used in the procedure can impact the success rate.
- Fertility Medications: Using fertility drugs to stimulate ovulation can improve the chances of success.
- Number of Cycles: Multiple attempts may increase the chances of pregnancy.
Is IUI Right for You?
IUI can be a great option for many couples dealing with infertility, but it’s important to discuss your unique situation with your doctor. IUI is most effective for people with specific fertility issues, such as mild male infertility or ovulatory disorders. If you have more complex issues, such as severe male infertility or blocked fallopian tubes, your doctor may recommend more advanced treatments like in vitro fertilization (IVF).
Pros of IUI
- Less Invasive: Compared to IVF, IUI is a less invasive procedure.
- Cost-Effective: IUI is typically more affordable than other fertility treatments.
- Convenient: The procedure is quick, and most women recover fast.
Cons of IUI
- Lower Success Rates: Compared to IVF, IUI has lower success rates.
- Side Effects of Fertility Medications: Medications to stimulate ovulation can cause side effects, such as bloating, mood swings, and hot flashes.
IUI vs. IVF: What’s the Difference?
While both IUI and in vitro fertilization (IVF) are fertility treatments, they differ in complexity and cost. In IUI sperms are placed directly into the uterus. Whereas IVF involves fertilizing an egg outside the body and then transferring the embryo into the uterus. IVF has higher success rates but is more invasive and expensive.
IUI is often recommended as a first step for couples who are struggling to conceive but don’t have significant fertility issues. IVF may be considered if IUI fails after several cycles or if the couple faces more severe infertility challenges.
Conclusion
IUI can be an effective, affordable, and less invasive fertility treatment for many people. It’s important to carefully assess your fertility challenges and discuss your options with your doctor. With proper guidance and realistic expectations, understanding IUI could be the right step in your journey toward parenthood.